Sharp penile pain represents one of the most distressing urological symptoms that can affect men across all age groups. This acute discomfort can manifest suddenly during various activities, from urination and sexual intercourse to periods of rest, significantly impacting quality of life and psychological wellbeing. Understanding the underlying mechanisms behind sharp penile pain is crucial for proper diagnosis and treatment, as the causes range from minor inflammatory conditions to serious medical emergencies requiring immediate intervention. The complexity of penile anatomy, combined with its dual role in both urinary and reproductive functions, creates multiple pathways through which pain can develop, making accurate identification of the root cause essential for effective management.
Infectious urethritis and sexually transmitted pathogens
Infectious urethritis represents one of the most common causes of sharp penile pain, particularly affecting sexually active men. The inflammation of the urethral lining creates a burning, stabbing sensation that intensifies during urination and may persist as a throbbing ache. Bacterial and viral pathogens infiltrate the delicate urethral mucosa, triggering an inflammatory cascade that results in tissue swelling, increased sensitivity, and characteristic discharge patterns.
Chlamydia trachomatis urethral inflammation
Chlamydia trachomatis infection frequently presents as sharp, burning penile pain that accompanies urination, affecting approximately 1.7 million men annually in the United States alone. The intracellular bacterial pathogen targets columnar epithelial cells within the urethra, causing microscopic tissue damage and inflammatory responses. Patients typically experience a gradual onset of symptoms, beginning with mild discomfort that progressively intensifies over several days to weeks. The pain often radiates from the urethral opening throughout the entire penile shaft, creating a persistent aching sensation between urination episodes.
Laboratory diagnosis requires nucleic acid amplification testing of first-catch urine specimens, with sensitivity rates exceeding 95% for detecting chlamydial infections. Treatment protocols involve single-dose azithromycin or seven-day doxycycline regimens, with pain resolution typically occurring within 48-72 hours of antibiotic initiation. Untreated chlamydial urethritis can progress to epididymitis, causing severe testicular pain and potential fertility complications.
Neisseria gonorrhoeae acute urethritis
Gonococcal urethritis produces some of the most intense sharp penile pain experienced in infectious conditions, with symptoms typically appearing within 2-7 days following exposure. The gram-negative diplococcus bacterium rapidly colonises urethral tissues, producing purulent discharge and severe dysuria that patients describe as “razor-like” or “glass shards” during urination. Unlike chlamydial infections, gonococcal urethritis presents with more pronounced systemic symptoms, including fever and malaise in approximately 30% of cases.
The diagnostic approach combines clinical presentation assessment with gram staining of urethral discharge, revealing characteristic intracellular diplococci in polymorphonuclear leukocytes. Modern treatment protocols address increasing antibiotic resistance patterns, with dual therapy using ceftriaxone plus azithromycin becoming the standard approach. Pain management strategies during the acute phase include topical anaesthetic preparations and non-steroidal anti-inflammatory drugs to reduce urethral inflammation.
Herpes simplex virus penile lesions
Herpes simplex virus (HSV) infections create distinctive sharp, stabbing pain patterns associated with vesicular lesions on penile skin surfaces. Primary HSV outbreaks typically produce more severe pain than recurrent episodes, with patients experiencing intense burning sensations 24-48 hours before visible lesions appear. The viral replication within sensory nerve endings generates neuropathic pain characteristics, including hypersensitivity to light touch and clothing contact.
Prodromal symptoms often include tingling, itching, and sharp shooting pains along the penile shaft, particularly affecting the glans and foreskin regions. Antiviral therapy with acyclovir, valacyclovir, or famciclovir significantly reduces pain duration and lesion healing time when initiated within 72 hours of symptom onset. Topical lidocaine preparations provide temporary pain relief, whilst oral analgesics may be necessary for severe cases.
Trichomonas vaginalis male urogenital infection
Trichomoniasis in males frequently presents as sharp urethral pain with associated burning during urination, though many infections remain asymptomatic. The flagellated protozoan parasite adheres to urethral epithelium, causing mechanical irritation and inflammatory responses that generate acute pain sensations. Approximately 15-20% of infected males develop symptomatic urethritis, with pain intensities varying from mild discomfort to severe burning sensations.
Diagnosis relies on nucleic acid amplification testing or direct microscopic examination of urethral discharge, revealing motile trichomonads in positive cases. Single-dose metronidazole therapy effectively eliminates the infection, with pain resolution typically occurring within 24-48 hours. Partner treatment remains essential to prevent reinfection cycles, as sexual transmission rates approach 85% during unprotected intercourse with infected individuals.
Mechanical trauma and physical injury mechanisms
Physical trauma to penile structures can produce immediate, severe sharp pain through various mechanisms involving tissue disruption, nerve damage, and vascular compromise. The penis’s complex anatomy, including erectile tissues, fascial layers, and neurovascular bundles, makes it particularly vulnerable to mechanical injuries during sexual activity, accidents, and medical procedures. Understanding these trauma patterns helps clinicians recognise emergency situations requiring immediate surgical intervention to preserve penile function and prevent long-term complications.
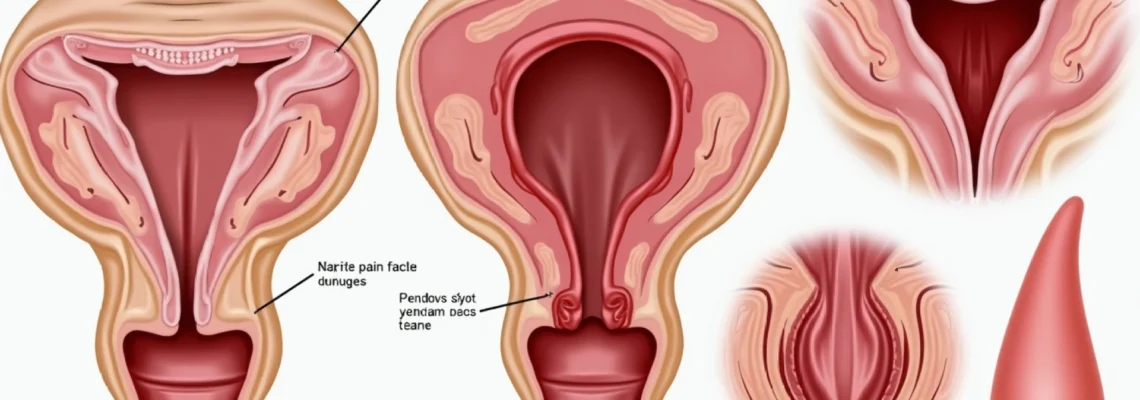
Penile fracture and tunica albuginea rupture
Penile fracture represents a true urological emergency characterised by rupture of the tunica albuginea surrounding the corpora cavernosa, typically occurring during forceful bending of the erect penis. Patients experience sudden, excruciating sharp pain accompanied by an audible “crack” or “pop,” followed by immediate detumescence and rapid swelling. The injury mechanism involves excessive force applied to the rigid erect penis, with sexual intercourse accounting for approximately 58% of cases, whilst masturbation contributes to 42% of incidents.
Clinical presentation includes severe pain, penile deformity, and characteristic “eggplant sign” appearance due to extensive haematoma formation beneath Buck’s fascia. Immediate surgical exploration and repair within 24 hours optimises functional outcomes, with delayed intervention associated with increased complications including erectile dysfunction, penile curvature, and painful erections. Surgical techniques involve degloving the penile shaft, evacuating haematomas, and primary repair of tunica albuginea defects using non-absorbable sutures.
Zipper entrapment and foreskin laceration
Zipper entrapment injuries create immediate sharp pain through mechanical compression and tissue ischaemia, particularly affecting prepubescent males and uncircumcised adults. The injury occurs when penile skin or foreskin becomes caught between zipper teeth, causing progressive tissue damage as swelling increases entrapment severity. Pain intensifies with any movement attempts, creating a cycle of anxiety and muscle tension that exacerbates tissue compression.
Management approaches vary depending on entrapment severity and zipper type, with options ranging from lubrication techniques using soap or mineral oil to surgical zipper removal under local anaesthesia. Prevention strategies include proper underwear use and careful attention during dressing, particularly in young children who may rush clothing procedures. Tetanus prophylaxis should be considered for significant lacerations, especially when metal zippers cause deeper tissue penetration.
Vigorous sexual activity frenulum tears
Frenulum tears during vigorous sexual activity produce sharp, localised pain accompanied by immediate bleeding from the highly vascularised tissue band connecting the glans to the foreskin. The frenulum’s limited elasticity makes it particularly susceptible to tearing during aggressive thrusting motions or inadequate lubrication conditions. Pain characteristics include initial sharp, cutting sensations followed by persistent burning and throbbing as inflammatory responses develop.
Most frenulum tears heal spontaneously with conservative management including local pressure for haemostasis, topical antibiotic ointments, and temporary sexual activity restriction. However, recurrent tearing may indicate frenulum breve, requiring surgical frenuloplasty to lengthen the restrictive tissue band. Recovery typically requires 2-3 weeks, with gradual return to normal sexual activity as tissue healing progresses and pain sensitivity decreases.
Catheter-related urethral trauma
Urethral catheterisation procedures can cause sharp penile pain through multiple mechanisms, including urethral stretching, mucosal abrasions, and balloon inflation trauma. Incorrect catheter sizing, inadequate lubrication, or forced insertion techniques contribute to tissue damage and subsequent pain development. The pain typically manifests as sharp, burning sensations during insertion, followed by persistent discomfort and spasmodic contractions around the catheter presence.
Preventive measures include proper catheter sizing, adequate lubrication with sterile gel, and gentle insertion techniques respecting natural urethral curvatures. Post-catheterisation pain management involves anticholinergic medications to reduce bladder spasms, topical anaesthetics for urethral discomfort, and appropriate analgesia based on pain severity. Long-term complications may include urethral stricture formation, requiring specialised urological intervention for resolution.
Inflammatory dermatological conditions
Inflammatory skin conditions affecting penile tissues frequently produce sharp, stabbing pain through various pathophysiological mechanisms involving immune system activation, tissue inflammation, and nerve sensitisation. These dermatological disorders can affect any part of the penile anatomy, from the glans and foreskin to the shaft skin, creating complex pain patterns that may be constant or triggered by specific activities such as urination, sexual contact, or clothing friction. The intimate location of these conditions often leads to delayed medical consultation, potentially worsening symptoms and complicating treatment approaches.
Balanitis and glans penis inflammation
Balanitis produces sharp, burning pain localised to the glans penis through inflammatory processes affecting the delicate mucosal surfaces beneath the foreskin. The condition results from bacterial overgrowth, candidal infections, or chemical irritation, creating tissue swelling, erythema, and hypersensitivity to touch or friction. Pain intensities vary from mild discomfort during urination to severe, constant burning sensations that interfere with daily activities and sleep patterns.
Bacterial balanitis typically presents with purulent discharge and more intense pain compared to candidal variants, which often feature white, cottage cheese-like discharge with associated itching. Treatment protocols depend on the underlying aetiology, ranging from topical antifungal preparations for candidal infections to antibiotic therapy for bacterial causes. Severe cases may require oral medications, particularly when infection spreads to surrounding tissues or becomes recurrent despite topical interventions.
Lichen sclerosus penile manifestations
Lichen sclerosus creates chronic sharp pain through progressive scarring and tissue atrophy affecting penile skin, particularly the glans and foreskin regions. This autoimmune condition produces characteristic white, porcelain-like patches that become increasingly painful as the disease progresses and tissue flexibility decreases. Patients experience sharp, stabbing pain during erections, sexual activity, and sometimes with simple touch or clothing friction.
The pathophysiology involves T-cell mediated inflammation leading to collagen deposition and tissue fibrosis, ultimately compromising normal penile function. Early intervention with potent topical corticosteroids can halt disease progression and reduce pain severity, though established scarring may require surgical intervention. Circumcision outcomes in advanced cases show significant pain reduction and improved quality of life, though timing of surgical intervention remains crucial for optimal results.
Contact dermatitis from latex allergens
Allergic contact dermatitis from latex exposure creates immediate sharp, burning pain through type IV hypersensitivity reactions affecting penile skin surfaces. Condom use represents the most common exposure route, though latex-containing lubricants, medical gloves during examinations, and other rubber products can trigger reactions. The pain develops within hours of exposure, beginning as mild irritation before progressing to intense burning and stabbing sensations.
Clinical presentation includes erythema, vesicle formation, and severe pruritus accompanied by sharp pain that worsens with scratching or friction. Diagnosis relies on detailed exposure history and patch testing to confirm latex sensitivity, though immediate symptom correlation with latex contact often provides clear evidence. Management involves complete latex avoidance, topical corticosteroids for acute inflammation, and alternative barrier methods for sexual activity to prevent recurrent reactions.
Candidal balanoposthitis presentations
Candidal balanoposthitis produces distinctive sharp pain patterns through fungal invasion of both glans and foreskin tissues, creating more extensive inflammation than simple balanitis. Candida albicans thrives in warm, moist environments beneath the foreskin, particularly in diabetic patients or those with compromised immune systems. The pain typically includes burning sensations during urination, sharp discomfort with foreskin retraction, and persistent aching between acute episodes.
Risk factors include diabetes mellitus, antibiotic therapy, immunosuppression, and poor hygiene practices that promote candidal overgrowth. Treatment approaches combine topical antifungal agents with systemic therapy for recurrent or severe cases, whilst addressing underlying predisposing factors to prevent reinfection. Preventive measures include proper hygiene education, blood glucose optimisation in diabetic patients, and consideration of circumcision for recurrent cases resistant to medical management.
Urological emergencies requiring immediate intervention
Several urological conditions producing sharp penile pain constitute true medical emergencies requiring immediate recognition and intervention to prevent irreversible tissue damage and preserve sexual function. These emergencies often present with characteristic pain patterns and associated symptoms that distinguish them from less urgent conditions, making rapid clinical assessment crucial for optimal patient outcomes. The time-sensitive nature of these conditions means that delayed diagnosis or treatment can result in permanent complications, including erectile dysfunction, tissue necrosis, and loss of reproductive function.
Priapism represents the most critical urological emergency affecting the penis, characterised by prolonged, painful erection lasting more than four hours without sexual stimulation. The condition occurs in two distinct forms: low-flow (ischaemic) priapism involving venous outflow obstruction, and high-flow (non-ischaemic) priapism resulting from arterial inflow increases following trauma. Low-flow priapism produces severe, progressive pain as corporal blood becomes deoxygenated and acidotic, creating tissue hypoxia that can lead to irreversible smooth muscle fibrosis within hours.
Emergency management protocols for low-flow priapism include immediate corporal blood aspiration and irrigation with sympathomimetic agents such as phenylephrine to restore normal detumescence. Pain management during these procedures requires appropriate anaesthesia, as the interventions themselves can be intensely uncomfortable. Surgical shunting procedures may be necessary when conservative measures fail, with various techniques available depending on the duration and severity of the episode. Early intervention within six hours offers the best prognosis for preserved erectile function, whilst delays beyond 24 hours significantly increase the risk of permanent impotence.
Paraphimosis creates another urological emergency through foreskin entrapment behind the glans penis, causing progressive swelling and vascular compromise that produces severe, escalating pain. The condition typically results from failure to reduce the foreskin following medical procedures, catheterisation, or sexual activity in patients with tight foreskins. As tissue swelling increases, the constricting band effect intensifies, creating a cycle of worsening oedema and increasing pain that can progress to tissue necrosis if left untreated.
The key to successful paraphimosis management lies in early recognition and prompt intervention, as delayed treatment significantly increases the complexity of reduction procedures and the risk of tissue loss.
Reduction techniques begin with topical anaesthesia and manual compression to decrease glans swelling, followed by gentle attempts at foreskin advancement over the glans. When conservative measures fail, emergency dorsal slit procedures or immediate circumcision may be necessary to relieve the constricting band and restore normal circulation. Post-reduction care includes anti-inflammatory medications, infection prophylaxis, and close monitoring for complications such as skin necrosis or recurrent episodes requiring definitive surgical intervention.
Neurological pain syndromes and nerve entrapment
Neurological conditions affecting penile innervation can produce distinctive sharp pain patterns that differ significantly from inflammatory
or infectious causes, often requiring specialised diagnostic approaches and targeted treatment strategies. These neurological pain syndromes involve dysfunction of the peripheral nerves that provide sensation to penile tissues, creating complex pain patterns that may be constant, intermittent, or triggered by specific stimuli. The pudendal nerve and its branches represent the primary neural pathways involved, though other nerve structures including the ilioinguinal and genitofemoral nerves can contribute to penile pain syndromes.Pudendal neuralgia affects the pudendal nerve as it travels through the pelvis, creating sharp, stabbing pain that radiates along the penile shaft and may extend to the perineum and rectum. The condition often results from nerve compression within Alcock’s canal or following pelvic surgery, cycling injuries, or prolonged sitting on hard surfaces. Patients describe the pain as electric shock-like sensations that worsen with sitting and improve when standing or lying down. The pain pattern typically follows the anatomical distribution of the pudendal nerve, affecting the ventral aspect of the penis and associated structures.Diagnosis of pudendal neuralgia requires careful clinical assessment combined with nerve conduction studies and sometimes diagnostic nerve blocks to confirm the source of symptoms. Treatment approaches include nerve blocks with local anaesthetics and corticosteroids, tricyclic antidepressants for neuropathic pain management, and anticonvulsant medications such as gabapentin or pregabalin. Physical therapy focusing on pelvic floor rehabilitation can provide significant symptom relief, whilst surgical decompression may be considered for refractory cases.Post-herpetic neuralgia following genital herpes infections creates persistent sharp pain along the distribution of affected sensory nerves, continuing long after the acute viral infection has resolved. The varicella-zoster virus or herpes simplex virus damages nerve fibres during the acute infection phase, leading to chronic neuropathic pain that can persist for months or years. Patients experience burning, stabbing, or electric shock-like sensations that may be triggered by light touch, clothing contact, or temperature changes.The pain intensity in post-herpetic neuralgia often exceeds that experienced during the acute infection, significantly impacting quality of life and sexual function. Early antiviral therapy during acute herpes episodes may reduce the risk of developing post-herpetic neuralgia, though prevention is not always achievable. Management strategies include topical anaesthetics such as lidocaine patches, systemic neuropathic pain medications, and sometimes interventional procedures including nerve blocks or radiofrequency ablation for severe cases resistant to conservative treatment.
Diagnostic evaluation and clinical assessment protocols
Accurate diagnosis of sharp penile pain requires systematic clinical evaluation incorporating detailed history taking, comprehensive physical examination, and appropriate laboratory or imaging studies. The diverse range of potential causes necessitates a methodical approach that considers both common conditions and rare but serious disorders requiring immediate intervention. Clinical assessment protocols must account for the sensitive nature of genital examinations whilst ensuring thorough evaluation to identify underlying pathology and guide appropriate treatment decisions.The diagnostic process begins with comprehensive history taking that explores pain characteristics, temporal patterns, associated symptoms, and potential precipitating factors. Clinicians should assess pain quality (sharp, burning, stabbing, or throbbing), location specificity, radiation patterns, and factors that aggravate or alleviate symptoms. Sexual history evaluation includes recent partner exposure, condom use, previous sexually transmitted infections, and any correlation between symptoms and sexual activity. Medical history review should identify diabetes, immunodeficiency conditions, previous urological procedures, and current medications that might predispose to penile pain conditions.Physical examination requires adequate lighting, patient positioning, and appropriate draping to maintain dignity whilst enabling thorough assessment. Visual inspection evaluates penile skin for lesions, discharge, swelling, or deformity, with particular attention to the glans, foreskin, and urethral meatus. Palpation assessment identifies areas of tenderness, masses, or induration that might indicate underlying pathology such as Peyronie’s disease plaques or inflammatory processes.Laboratory evaluation typically includes urinalysis with microscopy to identify infection markers, proteinuria, or haematuria that might indicate urological pathology. Nucleic acid amplification testing for sexually transmitted pathogens should be performed when infectious causes are suspected, with specimens collected according to appropriate protocols for optimal sensitivity. Blood glucose testing may be indicated when candidal infections are suspected or recurrent, as diabetes mellitus represents a significant risk factor for fungal overgrowth.Imaging studies play important roles in specific diagnostic scenarios, particularly when structural abnormalities or trauma are suspected. Penile ultrasound provides detailed assessment of corporal anatomy, identifying haematomas, fibrotic plaques, or vascular abnormalities that might not be apparent on physical examination alone. Doppler ultrasonography can evaluate penile blood flow patterns, particularly useful in assessing priapism or erectile dysfunction associated with pain symptoms.When neurological causes are suspected, specialised testing may include nerve conduction studies or electromyography to assess nerve function and identify specific sites of dysfunction. MRI imaging of the pelvis can identify nerve compression sites or structural abnormalities affecting pudendal nerve pathways, though such advanced imaging is typically reserved for complex cases not responding to initial treatment approaches.Urethroscopy may be indicated when urethral pathology is suspected, allowing direct visualisation of urethral mucosa and identification of strictures, foreign bodies, or inflammatory changes. This procedure requires appropriate anaesthesia and should be performed by experienced practitioners to minimise patient discomfort and potential complications.The diagnostic workup should be tailored to individual patient presentations, with urgent evaluation protocols implemented for emergency conditions such as priapism, paraphimosis, or suspected penile fracture. Risk stratification based on initial assessment guides the urgency and extent of diagnostic evaluation, ensuring that time-sensitive conditions receive immediate attention whilst avoiding unnecessary testing for straightforward diagnoses.Documentation of findings should be comprehensive and include pain scales, photographic documentation when appropriate and consented, and clear treatment plans with follow-up schedules. Patient education about findings, expected treatment responses, and warning signs requiring immediate medical attention forms an essential component of the diagnostic encounter, ensuring optimal outcomes and preventing complications through early recognition of treatment failures or disease progression.