The contraceptive implant Nexplanon represents one of the most effective long-acting reversible contraception methods available, with an efficacy rate exceeding 99%. However, the success and safety of this subdermal implant critically depend on proper insertion technique and optimal placement depth. When healthcare providers place the device too superficially, patients face significant risks ranging from immediate complications to long-term adverse outcomes. Understanding these risks becomes essential for both healthcare professionals and patients considering this contraceptive option.
Superficial placement occurs more frequently than many practitioners realise, with studies indicating that approximately 8-12% of implants may be positioned too close to the skin surface. This positioning error can lead to device visibility, increased infection rates, spontaneous extrusion, and aesthetic concerns. The implications extend beyond immediate complications, potentially affecting contraceptive efficacy and requiring premature removal or corrective procedures.
Nexplanon superficial insertion: clinical definition and depth parameters
Standard subdermal placement protocol: 8-10mm tissue depth requirements
The optimal placement of Nexplanon requires precise positioning within the subcutaneous tissue layer, specifically at a depth of 8-10 millimetres below the skin surface. This standardised depth ensures the implant sits comfortably within the hypodermis, surrounded by adequate fatty tissue that provides both protection and stability. The subcutaneous layer offers the ideal environment for hormone release whilst maintaining the device’s structural integrity throughout its three-year lifespan.
Healthcare providers must carefully assess tissue thickness during pre-insertion examination, particularly in patients with minimal subcutaneous fat. The insertion technique involves creating a subdermal tunnel using the provided applicator, with the healthcare professional maintaining constant awareness of needle depth and angle. Proper technique requires the practitioner to tent the skin whilst advancing the needle, ensuring the implant rests within the target tissue plane rather than approaching the skin surface or penetrating too deeply into muscle tissue.
Superficial implantation classification: less than 4mm skin distance
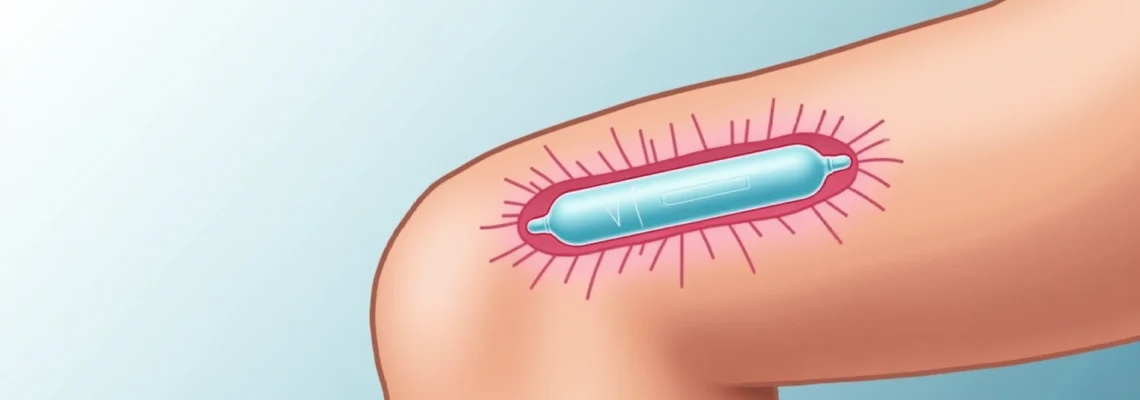
Medical literature defines superficial implantation as placement occurring at depths of less than 4 millimetres from the skin surface. At this shallow depth, the implant becomes readily visible through the skin, appearing as a distinct ridge or raised area along the upper arm. Patients can often see the device outline clearly, particularly when moving their arm or flexing muscles, which can cause significant cosmetic concerns and social discomfort.
This classification system helps healthcare providers assess implant positioning during follow-up appointments and determine appropriate management strategies. Superficial placement creates a cascade of potential complications that may necessitate early removal, replacement procedures, or additional medical interventions. The visibility factor alone prompts many patients to request premature device removal, despite satisfactory contraceptive function.
Anatomical considerations: upper arm tissue architecture and fascial layers
The upper arm’s anatomical structure comprises several distinct layers that influence implant placement success. The epidermis and dermis form the superficial skin layers, followed by the subcutaneous tissue containing adipose cells and connective tissue. Beneath this lies the deep fascia, which surrounds the underlying muscle groups. Understanding these anatomical landmarks enables healthcare providers to position the implant within the optimal tissue plane.
Individual anatomical variations significantly impact insertion technique requirements. Patients with limited subcutaneous fat, including athletes, elderly individuals, or those with low body mass index, present particular challenges for achieving adequate placement depth. The tissue architecture in these patients may require modified insertion angles or alternative placement sites to ensure appropriate positioning. Healthcare providers must adapt their technique based on individual patient anatomy rather than following a standardised approach for all cases.
Palpability index: visual and tactile assessment criteria
The palpability index provides a standardised method for assessing implant positioning immediately following insertion and during follow-up appointments. Properly placed implants should be easily palpable along their entire length whilst remaining invisible to visual inspection. Healthcare providers use a systematic approach involving gentle pressure along the implant site to confirm appropriate positioning and detect any areas of concern.
Superficially placed implants often demonstrate excessive palpability, with the device easily visible through the skin or creating prominent skin elevation. The tactile assessment reveals the implant sits too close to the surface when patients can feel the device’s edges distinctly or when minimal pressure is required for palpation. This assessment becomes crucial for identifying positioning errors that may require corrective intervention or enhanced monitoring protocols.
Immediate complications associated with superficial nexplanon placement
Skin erosion and ulceration: tissue necrosis risk factors
Superficial implant placement creates significant pressure against the overlying skin, potentially leading to tissue erosion and ulceration. The constant pressure from the rigid implant against thin skin layers can compromise local blood circulation, resulting in tissue hypoxia and eventual necrosis. This process typically develops gradually over weeks to months, beginning with skin thinning and progressing to partial-thickness erosions before potential full-thickness ulceration occurs.
Several factors increase the risk of skin erosion in superficially placed implants. Patients with diabetes, peripheral vascular disease, or compromised immune systems face elevated risks due to impaired wound healing capabilities. Additionally, individuals who engage in activities causing repetitive pressure or friction against the implant site, such as weightlifting or contact sports, may experience accelerated tissue breakdown. The inflammatory response triggered by the foreign body presence becomes more pronounced when the device sits closer to the skin surface.
Healthcare providers must monitor patients with superficially placed implants closely for early signs of skin compromise, including persistent redness, skin thinning, or patient reports of increasing tenderness at the implant site.
Implant extrusion mechanisms: spontaneous device migration patterns
Spontaneous extrusion represents one of the most concerning complications associated with superficial implant placement. The body’s natural healing response involves encapsulating foreign objects with fibrous tissue, but when an implant sits too close to the skin surface, this process may instead push the device towards the skin surface rather than stabilising it within the subcutaneous tissue. The extrusion process typically occurs gradually, with the implant slowly migrating through tissue planes until it breaches the skin surface.
The extrusion mechanism involves several biological processes, including inflammatory cell recruitment, collagen deposition, and tissue remodelling. When these processes occur in the context of inadequate tissue coverage, they may facilitate device migration rather than stable encapsulation. Patients experiencing implant extrusion often report increasing visibility of the device, skin tenting, or the sensation that the implant is “moving” beneath the skin. Complete extrusion results in device loss and immediate contraceptive failure, requiring emergency contraceptive measures and alternative contraception methods.
Infection susceptibility: bacterial colonisation and biofilm formation
Superficially placed implants demonstrate increased susceptibility to bacterial colonisation and subsequent infection development. The proximity to the skin surface creates easier pathways for bacterial migration from the skin microbiome to the implant site. Common skin organisms, including Staphylococcus epidermidis and Staphylococcus aureus, can establish persistent infections around superficially placed devices, particularly when biofilm formation occurs on the implant surface.
Biofilm development represents a particularly challenging aspect of implant-associated infections. Bacteria within biofilms demonstrate increased antibiotic resistance and enhanced persistence compared to planktonic organisms. The biofilm matrix protects bacterial communities from immune system clearance and antimicrobial treatments, often necessitating implant removal for successful infection resolution. Patients with superficial implants who develop infections may require prolonged antibiotic courses, surgical drainage procedures, or premature device removal to achieve infection control.
Aesthetic deformity: visible implant outline and skin discolouration
The cosmetic impact of superficial implant placement extends beyond simple visibility concerns. Patients often experience significant psychological distress related to the device’s prominent appearance, particularly in social or intimate situations where arm exposure occurs. The visible implant outline may create a permanent raised ridge along the upper arm, accompanied by skin discolouration or texture changes that persist even after device removal.
Long-term aesthetic consequences may include hyperpigmentation or hypopigmentation at the implant site, skin atrophy, or permanent scarring. These changes result from chronic pressure effects, inflammatory responses, and altered local blood flow patterns. The psychological impact of these aesthetic changes should not be underestimated, as many patients report decreased quality of life, social anxiety, or relationship difficulties related to the visible implant appearance. Healthcare providers must discuss these potential outcomes during pre-insertion counselling to ensure informed consent.
Long-term medical consequences of inadequate insertion depth
The long-term medical implications of superficial Nexplanon placement extend far beyond immediate complications, creating ongoing health risks that may persist throughout the device’s intended lifespan. Chronic inflammatory responses develop around superficially placed implants, leading to persistent tissue irritation and potential systemic inflammatory markers elevation. This prolonged inflammation can compromise local tissue integrity and create favourable conditions for secondary complications such as chronic pain syndromes or nerve sensitisation.
Hormonal delivery patterns may also be altered in superficially placed implants, though research on this aspect remains limited. The reduced tissue coverage could potentially affect hormone diffusion patterns, leading to irregular serum levels of etonogestrel. While contraceptive efficacy generally remains maintained, patients may experience increased side effects related to hormone fluctuations, including irregular bleeding patterns, mood changes, or other hormonal symptoms. The bioavailability of the contraceptive hormone may be influenced by the altered tissue environment surrounding superficial implants.
Nerve irritation represents another significant long-term consequence of inadequate insertion depth. Superficial implants may create chronic pressure against cutaneous nerve branches, leading to persistent numbness, tingling, or hypersensitivity in the surrounding skin areas. These neurological symptoms can significantly impact quality of life and may require specialised pain management approaches. In severe cases, nerve damage may be permanent, persisting even after implant removal and requiring ongoing medical management.
The financial implications of managing superficial implant complications can be substantial, including costs associated with early removal procedures, replacement devices, treatment of complications, and potential legal liabilities for healthcare providers.
Device integrity concerns also arise with superficial placement, as the increased mechanical stress from proximity to the skin surface may compromise the implant’s structural stability. Reports of device fracture or fragmentation occur more frequently in superficially placed implants, potentially complicating removal procedures and creating additional health risks. Fragmented implants may require surgical exploration for complete removal, increasing patient morbidity and healthcare costs significantly.
Diagnostic assessment protocols for superficial nexplanon detection
High-frequency ultrasound evaluation: 10-15 MHz transducer applications
High-frequency ultrasound imaging using 10-15 MHz transducers provides the most accurate non-invasive method for assessing implant depth and positioning. This imaging modality offers excellent resolution for superficial structures, allowing healthcare providers to measure the precise distance between the implant surface and overlying skin. The ultrasound examination can identify implants positioned at depths of less than 4 millimetres with high accuracy, enabling early intervention before complications develop.
The ultrasound protocol involves systematic scanning along the entire implant length, documenting depth measurements at multiple points to identify any areas of particular concern. Healthcare providers trained in ultrasound techniques can also assess surrounding tissue characteristics, identifying signs of inflammation, fluid collection, or other complications associated with superficial placement. This imaging approach proves particularly valuable in patients with difficult-to-palpate implants or those presenting with symptoms suggestive of malposition.
Clinical examination techniques: pinch test and manual palpation methods
The pinch test represents a simple but effective clinical assessment tool for identifying superficial implant placement during routine examinations. This technique involves gently pinching the skin over the implant site and measuring the thickness of tissue that can be grasped. When less than 4 millimetres of tissue can be pinched over the implant, superficial placement should be suspected and further evaluation considered. The pinch test provides immediate feedback about implant positioning without requiring specialised equipment or extensive training.
Manual palpation techniques complement the pinch test by assessing implant mobility, surrounding tissue characteristics, and patient comfort during examination. Properly positioned implants should be easily palpable but not visible, with adequate surrounding tissue providing cushioning against pressure. Superficially placed implants often demonstrate reduced mobility, increased visibility during palpation, or patient discomfort when pressure is applied. Healthcare providers should document these findings systematically and consider additional imaging if abnormal positioning is suspected.
Radiological imaging: x-ray and MRI contraindication considerations
Plain radiography can identify Nexplanon implants due to the radiopaque barium sulphate incorporated into the device design. However, X-ray imaging provides limited information about soft tissue depth relationships and is generally not recommended as a primary assessment tool for positioning evaluation. The two-dimensional nature of plain radiographs makes accurate depth assessment challenging, particularly in patients with variable tissue thickness or overlapping anatomical structures.
Magnetic resonance imaging (MRI) is generally contraindicated for Nexplanon assessment due to potential heating effects and image artifact production. The implant contains metallic components that can create significant imaging artifacts, compromising diagnostic quality whilst potentially posing safety risks to patients. Healthcare providers should avoid MRI imaging for implant assessment unless absolutely necessary for other medical conditions, and must inform radiologists about implant presence before any MRI procedures. Alternative imaging modalities such as ultrasound provide superior diagnostic information for implant positioning assessment without the associated risks of MRI examination.
Corrective management strategies for superficially placed implants
The management of superficially placed Nexplanon implants requires a individualised approach based on symptom severity, complication presence, and patient preferences. Immediate removal may be necessary in cases involving active complications such as infection, erosion, or threatened extrusion. However, asymptomatic superficial implants may be managed conservatively with enhanced monitoring protocols, particularly if the patient desires to maintain contraceptive coverage and removal would create significant inconvenience or contraceptive gaps.
When removal becomes necessary, healthcare providers must employ specialised techniques to safely extract superficially placed implants whilst minimising tissue trauma and scarring. The proximity to the skin surface can actually simplify the removal process in some cases, but may also increase the risk of skin perforation or inadequate healing. Local anaesthetic administration requires careful consideration of injection depth and volume to provide adequate pain control without compromising tissue planes or creating additional complications during the procedure.
Replacement procedures following superficial implant removal present unique challenges, as the previous insertion site may not be suitable for immediate reimplantation. Healthcare providers must assess tissue integrity, inflammatory status, and healing progression before considering replacement device insertion. Alternative insertion sites, such as the contralateral arm or different locations within the same arm, may be necessary to ensure optimal positioning and prevent recurrent complications. The replacement timing should allow adequate tissue healing whilst maintaining contraceptive coverage through alternative methods.
Patient counselling becomes crucial during corrective management, as individuals may experience anxiety about removal procedures, concerns about contraceptive gaps, or disappointment about device failure requiring intervention.
Follow-up protocols for patients who have experienced superficial implant placement require enhanced surveillance to monitor for recurrent complications or problems with replacement devices. These patients may benefit from more frequent clinical assessments, ultrasound evaluations, or specialist referrals to ensure optimal outcomes. Healthcare providers should maintain detailed documentation of complications, interventions, and outcomes to contribute to quality improvement efforts and inform future insertion practices.
Prevention protocols: optimal insertion technique and training requirements
Preventing superficial implant placement requires comprehensive training programmes that emphasise proper insertion technique, anatomical knowledge, and complication recognition. Healthcare providers must demonstrate competency in identifying appropriate insertion sites, assessing patient anatomy, and adapting techniques based on individual patient characteristics. Standardised training protocols should include hands-on practice with insertion devices, anatomical models, and supervised clinical experience before independent practice authorisation.
The insertion technique protocol begins with careful patient positioning, ensuring the non-dominant arm is flexed appropriately with the hand positioned behind the head. This positioning optimises access to the insertion site whilst deflecting anatomical structures away from the needle path. Healthcare providers must identify anatomical landmarks precisely, marking the insertion site 8-10 centimetres from the medial epicondyle and ensuring adequate distance from neurovascular structures. The marking technique should account for individual patient anatomy variations and tissue thickness assessment.
Quality assurance measures should include regular competency assessments, complication tracking systems, and continuous education programmes addressing new techniques or safety updates. Healthcare facilities offering implant services must maintain proper equipment, including ultrasound capabilities for positioning confirmation when indicated. Peer review
processes should evaluate not only technical insertion skills but also patient communication abilities and complication management knowledge. Regular updates on device modifications, new safety protocols, or emerging complications ensure healthcare providers maintain current expertise throughout their practice careers.
Pre-insertion assessment protocols play a crucial role in preventing superficial placement by identifying high-risk patients and selecting appropriate insertion sites. Healthcare providers should systematically evaluate patient anatomy, including subcutaneous tissue thickness, muscle definition, and vascular anatomy visibility. Patients with minimal subcutaneous fat, previous surgical scars, or anatomical abnormalities may require modified insertion approaches or alternative contraceptive methods. The assessment should also include discussion of patient expectations, lifestyle factors, and aesthetic concerns that might influence insertion site selection.
Documentation requirements for implant insertion procedures should include detailed anatomical assessments, insertion technique modifications, immediate post-insertion findings, and patient education provided. This comprehensive documentation serves multiple purposes, including medicolegal protection, quality improvement tracking, and clinical research contributions. Healthcare providers must also establish clear protocols for follow-up care, complication reporting, and patient communication regarding warning signs that might indicate positioning problems or developing complications.
Establishing robust training programmes and quality assurance measures represents the most effective strategy for preventing superficial implant placement and ensuring optimal patient outcomes throughout the contraceptive device lifespan.
Continuing education requirements should mandate regular skill updates, complication case reviews, and participation in professional development activities related to implant contraception. Healthcare systems must invest in proper training infrastructure, including simulation equipment, expert mentorship programmes, and ongoing competency verification systems. The investment in prevention through comprehensive training proves far more cost-effective than managing complications resulting from inadequate insertion technique or insufficient provider preparation.
Patient education initiatives complement provider training by ensuring individuals understand the importance of proper implant positioning and can participate actively in post-insertion monitoring. Patients should receive clear instructions about normal healing expectations, warning signs requiring immediate medical attention, and the importance of follow-up appointments. Educational materials should emphasise that visible implant outlines or excessive palpability may indicate positioning problems requiring professional evaluation, empowering patients to seek appropriate care when concerns arise.
Technology integration, including point-of-care ultrasound capabilities and digital training resources, enhances both provider competency and patient safety outcomes. Healthcare facilities should consider implementing ultrasound-guided insertion techniques for high-risk patients or providers developing insertion skills. Digital training platforms can provide standardised education delivery, competency tracking, and continuous professional development opportunities that support optimal insertion practices across diverse healthcare settings.
Regulatory oversight and accreditation programmes ensure healthcare providers meet minimum competency standards before offering implant services independently. These programmes should include theoretical knowledge assessment, practical skill demonstration, and ongoing quality monitoring to maintain certification validity. Professional organisations play a crucial role in establishing and maintaining these standards, providing resources for healthcare providers, and advocating for patient safety improvements within the field of contraceptive implant services.
Quality improvement initiatives should systematically track insertion outcomes, complication rates, and patient satisfaction measures to identify areas for improvement and best practice development. Healthcare systems implementing implant services must establish robust data collection systems that support continuous improvement efforts whilst maintaining patient confidentiality and regulatory compliance. Regular case reviews, outcome analysis, and practice modification based on evidence-based findings ensure optimal patient care delivery and minimise the risk of superficial placement complications.