Indentations or depressions in the shin bone represent a complex medical phenomenon that can arise from various underlying conditions and traumatic events. The tibia, being the largest weight-bearing bone in the lower leg, experiences significant mechanical stress during daily activities and sporting endeavours. When abnormal indentations develop on the shin bone surface, they often signal underlying pathological processes that require careful evaluation and appropriate management. Understanding the multifaceted nature of tibial indentation causes enables healthcare professionals to provide targeted treatment approaches and helps patients recognise when medical intervention becomes necessary.
Anatomical structure and function of the tibial bone
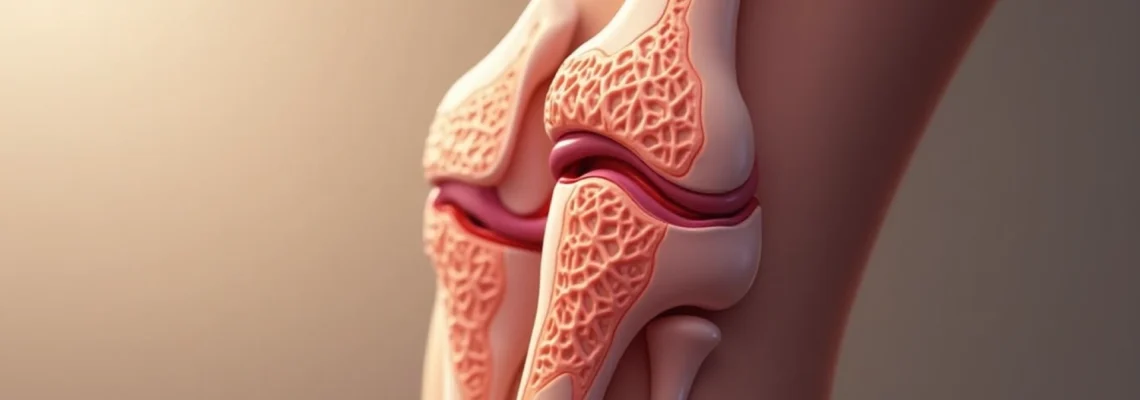
The tibia serves as the primary load-bearing bone of the lower leg, extending from the knee joint to the ankle. This robust structure consists of a proximal end that articulates with the femur, a long shaft known as the diaphysis, and a distal end that forms part of the ankle joint. The tibial shaft features a distinctive triangular cross-section with three distinct borders: the anterior border, which lies directly beneath the skin and creates the palpable shin ridge, the medial border, and the interosseous border that faces the fibula.
Medial tibial stress syndrome and cortical bone adaptations
Medial tibial stress syndrome , commonly referred to as shin splints, represents one of the most frequent causes of tibial surface irregularities in athletes. This condition develops when repetitive mechanical loading exceeds the bone’s adaptive capacity, leading to microscopic bone damage and subsequent remodelling responses. The medial aspect of the tibia becomes particularly vulnerable due to the attachment points of various muscles and fascial structures that generate significant tensile forces during running and jumping activities.
Research indicates that athletes who rapidly increase training intensity or duration face heightened risk for developing stress-related tibial changes. The bone responds to excessive loading by initiating osteoblastic activity, which can create temporary surface irregularities as new bone formation occurs. Cortical bone adaptations manifest as localised thickening or remodelling that may present as subtle indentations or raised areas along the tibial shaft.
Periosteal membrane inflammation and tibial ridge morphology
The periosteum, a thin membrane covering the bone surface, plays a crucial role in bone health and repair mechanisms. Inflammatory processes affecting the periosteal membrane can lead to visible and palpable changes in tibial contour. Direct trauma to the shin often damages the periosteum, causing localised bleeding and subsequent haematoma formation beneath this protective layer. The resulting inflammatory response can create temporary indentations as the accumulated blood clot organises and resolves.
Chronic periosteal inflammation, whether from repetitive trauma or systemic inflammatory conditions, may result in permanent alterations to tibial surface morphology. The periosteum contains numerous blood vessels and nerve fibres, making it highly responsive to mechanical stress and chemical irritants. When persistently inflamed, the periosteal membrane may thicken irregularly, creating areas of apparent depression relative to adjacent raised regions.
Anterior tibial compartment pressure distribution
The anterior compartment of the lower leg houses several important muscles, including the tibialis anterior, extensor hallucis longus, and extensor digitorum longus. Increased pressure within this compartment can affect the overlying soft tissues and create the appearance of tibial indentation. Compartment syndrome , whether acute or chronic, alters normal tissue architecture and may compress superficial structures against the underlying bone surface.
Chronic exertional compartment syndrome particularly affects endurance athletes and military personnel who engage in prolonged running activities. The increased compartmental pressure during exercise can gradually modify soft tissue contours, making certain areas of the tibia appear more prominent or depressed relative to surrounding regions. This condition often requires specialised testing to confirm the diagnosis and determine appropriate treatment strategies.
Osteoblastic activity and bone remodelling processes
Normal bone remodelling involves a delicate balance between osteoblastic bone formation and osteoclastic bone resorption. Disruptions to this equilibrium can result in localised areas of increased or decreased bone density, potentially creating surface irregularities. Osteoblastic activity increases in response to mechanical stress, hormonal influences, and various metabolic factors that affect calcium homeostasis and bone metabolism.
Certain medications, particularly corticosteroids and some chemotherapy agents, can interfere with normal bone remodelling processes. Long-term use of these substances may lead to irregular bone formation patterns that manifest as surface depressions or protrusions along the tibial shaft. Understanding these medication-related effects becomes particularly important when evaluating patients with unexplained tibial contour changes.
Traumatic injuries causing tibial indentation
Traumatic events represent the most common immediate cause of tibial indentation, ranging from minor contusions to severe fractures requiring surgical intervention. The anterior location of the tibia makes it particularly vulnerable to direct impact injuries during sporting activities, occupational accidents, and motor vehicle collisions. The severity of resulting indentation depends on the force magnitude, impact duration, and the specific anatomical structures involved in the traumatic event.
Direct impact trauma and haematoma formation
Direct blows to the shin bone frequently occur in contact sports such as football, rugby, and martial arts. The immediate consequence involves damage to the periosteum and surrounding soft tissues, leading to localised bleeding and haematoma development . The accumulated blood beneath the periosteum creates a palpable mass that initially appears as a raised area but may subsequently organise into a depression as the clot resolves and scar tissue forms.
Direct trauma to the shin bone can damage the periosteum, causing a collection of blood underneath that forms a haematoma and triggers an inflammatory response to heal the affected area.
The healing process following direct impact trauma involves several distinct phases. Initially, inflammatory mediators flood the injured area, causing pain, swelling, and localised warmth. Subsequently, fibroblasts migrate to the injury site and begin depositing collagen to repair damaged tissues. This repair process may result in irregular tissue architecture that creates permanent surface contour changes if not properly managed during the acute healing phase.
Stress fractures in athletes and military personnel
Stress fractures develop when repetitive loading exceeds the bone’s ability to adapt through normal remodelling processes. These injuries commonly affect runners, dancers, and military recruits who engage in high-impact activities without adequate conditioning periods. The tibial shaft represents one of the most frequent locations for stress fracture development, particularly along the posteromedial border where tensile forces concentrate during running activities.
Early stress fracture development may manifest as subtle surface irregularities before progressing to complete cortical disruption. Athletes often describe a gradual onset of pain that initially improves with rest but progressively worsens with continued activity. The bone attempts to repair microscopic damage through increased osteoblastic activity, which can temporarily create surface irregularities as new bone formation occurs in response to the ongoing stress.
Compartment syndrome secondary to tibial trauma
Severe tibial trauma can precipitate acute compartment syndrome, a surgical emergency requiring immediate intervention to prevent permanent tissue damage. The increased pressure within fascial compartments compresses blood vessels and nerves, potentially leading to muscle necrosis and permanent functional deficits. Post-traumatic compartment syndrome may result in permanent contour changes as damaged muscles undergo fibrosis and scarring processes.
Chronic compartment syndrome develops more gradually and often affects athletes engaged in repetitive lower leg activities. The persistent elevation in compartmental pressure can modify tissue architecture over time, creating areas of apparent tibial depression as surrounding muscles undergo adaptive changes. This condition requires specialised pressure monitoring techniques for definitive diagnosis and may necessitate surgical fasciotomy for symptom resolution.
Post-surgical tibial deformities and hardware complications
Surgical procedures involving the tibia can result in permanent contour changes due to bone removal, hardware placement, or healing complications. Plate fixation for tibial fractures may create palpable prominences or depressions, particularly in thin individuals where hardware lies close to the skin surface. Hardware-related complications such as screw loosening or plate breakage can also modify tibial contour and may require revision surgery.
Bone grafting procedures, whether autologous or synthetic, can create irregular surface contours as the graft material integrates with native bone tissue. The remodelling process following bone grafting may take several months to complete, during which time surface irregularities may be prominent. Understanding these normal healing processes helps differentiate expected post-surgical changes from pathological complications requiring intervention.
Pathological conditions associated with shin bone depression
Various systemic and localised pathological conditions can contribute to tibial contour abnormalities beyond traumatic causes. Metabolic bone diseases such as osteoporosis and osteomalacia affect bone density and structural integrity, potentially leading to deformation under normal physiological loads. Paget’s disease represents a particularly notable condition that can cause dramatic changes in bone architecture, including areas of apparent depression relative to regions of excessive bone formation.
Infectious processes affecting the tibia can result in permanent contour changes through direct bone destruction or secondary inflammatory responses. Osteomyelitis, particularly when involving the anterior tibial cortex, may create areas of bone loss that manifest as surface depressions. Chronic infections often require prolonged antibiotic treatment and may necessitate surgical debridement of affected bone tissue, further contributing to contour irregularities.
Neoplastic conditions, whether primary bone tumours or metastatic lesions, can significantly alter tibial architecture. Benign tumours such as osteoid osteoma may create localised areas of increased bone formation, making adjacent regions appear relatively depressed. Malignant lesions often cause bone destruction that results in obvious contour defects requiring oncological evaluation and treatment planning.
Vascular conditions affecting the lower extremity can also contribute to apparent tibial indentation through secondary effects on surrounding soft tissues. Chronic venous insufficiency and lymphoedema can cause persistent swelling that alters the relationship between bone and overlying tissues. In severe cases, chronic oedema may lead to skin and subcutaneous tissue changes that create the appearance of tibial depression even when the underlying bone remains normal.
Diagnostic imaging techniques for tibial abnormalities
Accurate diagnosis of tibial indentation causes requires systematic evaluation using appropriate imaging modalities tailored to the suspected underlying pathology. Plain radiographs serve as the initial imaging study for most tibial complaints, providing excellent visualisation of bone architecture, fracture patterns, and gross structural abnormalities. Weight-bearing radiographs offer particular value when assessing deformity correction or load distribution patterns that may contribute to surface irregularities.
Magnetic resonance imaging provides superior soft tissue contrast and enables detailed evaluation of bone marrow, periosteal changes, and surrounding muscle architecture. This modality proves particularly valuable when assessing stress fractures, osteomyelitis, or soft tissue masses that may contribute to apparent tibial indentation. MRI sequences can differentiate between various pathological processes and guide appropriate treatment planning based on specific tissue characteristics.
Computed tomography excels at demonstrating cortical bone detail and proves invaluable when evaluating complex fracture patterns or planning surgical interventions. Three-dimensional reconstruction capabilities allow comprehensive assessment of bone contour abnormalities and facilitate preoperative planning for corrective procedures. CT angiography may be indicated when vascular compromise is suspected in cases of severe trauma or compartment syndrome.
Advanced imaging techniques enable healthcare professionals to differentiate between various causes of tibial indentation and develop targeted treatment strategies based on specific pathological findings.
Bone scintigraphy demonstrates metabolic activity and proves particularly sensitive for detecting stress fractures, infections, and metastatic disease. This nuclear medicine technique can identify pathological processes before structural changes become apparent on conventional radiographs. SPECT-CT imaging combines the metabolic information from bone scintigraphy with the anatomical detail of computed tomography, providing comprehensive evaluation of complex tibial abnormalities.
Treatment protocols for tibial indentation management
Treatment approaches for tibial indentation vary significantly depending on the underlying cause, severity of symptoms, and patient-specific factors such as age, activity level, and comorbidities. Conservative management strategies often prove effective for minor traumatic injuries and stress-related conditions, while severe trauma or pathological processes may require surgical intervention. Evidence-based protocols emphasise early accurate diagnosis to guide appropriate treatment selection and optimise long-term outcomes.
Conservative management with RICE protocol implementation
The RICE protocol—rest, ice, compression, and elevation—remains the cornerstone of acute tibial injury management. This approach proves particularly effective for minor contusions and early-stage stress reactions where tissue damage remains limited. Rest periods allow natural healing processes to proceed without additional mechanical stress that might exacerbate tissue damage or delay recovery.
Ice application during the acute phase helps control inflammation and provides pain relief through local anaesthetic effects. Compression garments or elastic bandages can minimise swelling and provide proprioceptive feedback that may reduce secondary injury risk. Elevation of the affected limb above heart level when possible facilitates venous drainage and reduces gravitational pooling of inflammatory exudate that can impede healing processes.
Physiotherapy interventions and biomechanical correction
Physiotherapy treatment plays a crucial role in managing tibial indentation conditions, particularly those related to overuse or biomechanical factors. Initial interventions focus on pain control and inflammation reduction using modalities such as ultrasound, electrical stimulation, and manual therapy techniques. Progressive loading protocols help restore normal tissue architecture while minimising re-injury risk during the healing phase.
Biomechanical assessment identifies contributing factors such as abnormal gait patterns, muscle imbalances, or training errors that may predispose to tibial stress injuries. Corrective exercises targeting specific muscle groups can address these underlying issues and reduce recurrence risk. Gait retraining programmes prove particularly valuable for runners experiencing stress-related tibial problems, often involving modifications to foot strike patterns and cadence optimisation.
Advanced physiotherapy techniques include dry needling, soft tissue mobilisation, and graduated strength training programmes tailored to individual patient needs. Return-to-activity protocols ensure adequate tissue healing before resuming high-impact activities that might precipitate symptom recurrence. Load management strategies help athletes maintain fitness levels while allowing adequate recovery time for damaged tissues.
Surgical reconstruction techniques for severe cases
Severe tibial indentation resulting from fractures, bone loss, or failed conservative treatment may require surgical intervention to restore normal anatomy and function. Open reduction and internal fixation represents the standard approach for displaced fractures causing significant contour abnormalities. Modern plate and screw systems provide stable fixation while minimising soft tissue disruption and preserving blood supply to healing bone.
Bone grafting procedures may be necessary when significant bone loss creates unacceptable contour defects or compromises structural integrity. Autologous bone graft harvested from the iliac crest provides excellent biological properties, while synthetic bone substitutes offer advantages in terms of unlimited availability and reduced donor site morbidity. Reconstruction techniques must balance functional restoration with aesthetic considerations, particularly in visible areas such as the anterior tibial border.
Complex cases involving extensive bone loss or infection may require staged procedures incorporating temporary external fixation, aggressive debridement, and delayed reconstruction using vascularised bone grafts. Microsurgical techniques enable transfer of healthy bone and soft tissue from distant sites, providing viable options for challenging reconstructive scenarios. Distraction osteogenesis represents an alternative approach for addressing length discrepancies or contour abnormalities through controlled bone lengthening processes.
Pharmaceutical management of inflammatory responses
Anti-inflammatory medications play a supportive role in managing acute tibial injuries and certain chronic conditions contributing to bone contour abnormalities. Non-steroidal anti-inflammatory drugs (NSAIDs) provide effective pain relief and help control inflammatory responses that may impede healing. However, prolonged NSAID use requires careful monitoring due to potential adverse effects on bone healing and gastrointestinal function.
Topical anti-inflammatory preparations offer localised treatment benefits with reduced systemic exposure compared to oral medications. These formulations prove particularly useful for superficial conditions affecting the tibial periosteum or surrounding soft tissues. Corticosteroid injections may be considered for specific conditions such as chronic compartment syndrome or refractory inflammatory processes, though their use requires careful consideration of potential complications including tissue atrophy and delayed healing
risks.
Bisphosphonate medications, commonly prescribed for osteoporosis management, can occasionally contribute to atypical fracture patterns that may result in tibial contour abnormalities. These medications alter bone turnover rates and may predispose certain patients to stress fracture development, particularly with long-term use. Calcium and vitamin D supplementation often accompanies pharmaceutical interventions to optimise bone health and support natural healing processes.
Analgesic medications provide symptomatic relief during acute phases of tibial injury management. Acetaminophen offers effective pain control with minimal anti-inflammatory effects, making it suitable for patients requiring pain relief without potential interference with bone healing processes. Opioid medications may be necessary for severe acute pain but require careful monitoring and gradual tapering to prevent dependency issues and facilitate return to normal activities.
Prevention strategies and risk factor modification
Preventing tibial indentation involves addressing modifiable risk factors through lifestyle modifications, training adjustments, and environmental considerations. Primary prevention strategies focus on reducing injury risk before problems develop, while secondary prevention aims to prevent recurrence in individuals with previous tibial issues. Understanding individual risk profiles enables targeted interventions that can significantly reduce the likelihood of developing problematic tibial contour changes.
Training modification represents one of the most effective prevention strategies for athletes and active individuals. The “10% rule” recommends limiting weekly training increases to no more than 10% of the previous week’s volume, allowing adequate time for tissue adaptation without overwhelming repair mechanisms. Progressive loading protocols enable gradual conditioning that strengthens bone and surrounding tissues while minimising injury risk during the adaptation period.
Proper footwear selection plays a crucial role in preventing tibial stress injuries, particularly for runners and other athletes engaged in high-impact activities. Shoes should provide appropriate cushioning for individual foot types while maintaining adequate support for biomechanical alignment. Replacement schedules recommend changing running shoes every 300-500 miles to ensure continued shock absorption and support properties throughout the shoe’s functional lifespan.
Implementing comprehensive prevention strategies can reduce tibial injury risk by up to 70% in high-risk populations such as military recruits and endurance athletes.
Surface selection significantly influences tibial stress during running and walking activities. Softer surfaces such as grass, dirt trails, or synthetic tracks provide better shock absorption compared to concrete or asphalt surfaces. When softer surfaces are unavailable, alternating between different surface types can help distribute mechanical stress and reduce repetitive loading patterns that contribute to overuse injuries. Banking and camber considerations also influence tibial stress, with consistently running on banked surfaces potentially creating asymmetrical loading patterns.
Nutritional factors contribute to bone health and injury prevention through multiple mechanisms. Adequate calcium intake supports bone mineralisation and strength, while vitamin D ensures proper calcium absorption and bone metabolism. Protein consumption provides essential amino acids for tissue repair and bone matrix formation, with current recommendations suggesting 1.2-2.0 grams per kilogram of body weight for active individuals.
Cross-training activities help maintain cardiovascular fitness while reducing repetitive stress on the tibia and surrounding structures. Swimming, cycling, and elliptical training provide excellent cardiovascular benefits with minimal tibial loading, making them ideal alternatives during recovery periods or as supplementary activities. Strength training programs targeting the lower extremities can improve bone density and muscular support systems that help protect against tibial stress injuries.
Environmental considerations include adequate hydration, appropriate clothing for temperature regulation, and recognition of conditions that may increase injury risk. Dehydration can affect muscle function and coordination, potentially increasing fall risk and direct trauma exposure. Heat-related stress may compromise decision-making and increase fatigue levels that contribute to poor biomechanics and injury susceptibility.
Regular health monitoring through periodic medical evaluations can identify risk factors before they contribute to tibial problems. Bone density screening may be appropriate for individuals with multiple risk factors or previous stress fracture history. Biomechanical assessments can identify movement patterns that predispose to tibial stress and enable corrective interventions before injury occurs.
Sleep quality and recovery practices significantly influence tissue repair and adaptation processes essential for preventing overuse injuries. Adequate sleep duration and quality support growth hormone release and protein synthesis necessary for bone and soft tissue maintenance. Recovery modalities such as massage, stretching, and appropriate rest periods between training sessions optimise adaptation while minimising injury risk.
Understanding individual risk factors enables personalised prevention strategies that address specific predisposing conditions. Factors such as previous injury history, biomechanical abnormalities, training experience, and underlying health conditions all influence injury susceptibility. Risk stratification systems can help identify high-risk individuals who may benefit from enhanced prevention measures or modified activity recommendations.
Long-term prevention success requires consistent implementation of multiple strategies rather than relying on single interventions. Regular reassessment of prevention protocols ensures continued effectiveness as individual circumstances change over time. Education programs help athletes, coaches, and healthcare providers recognise early warning signs and implement appropriate modifications before serious problems develop.