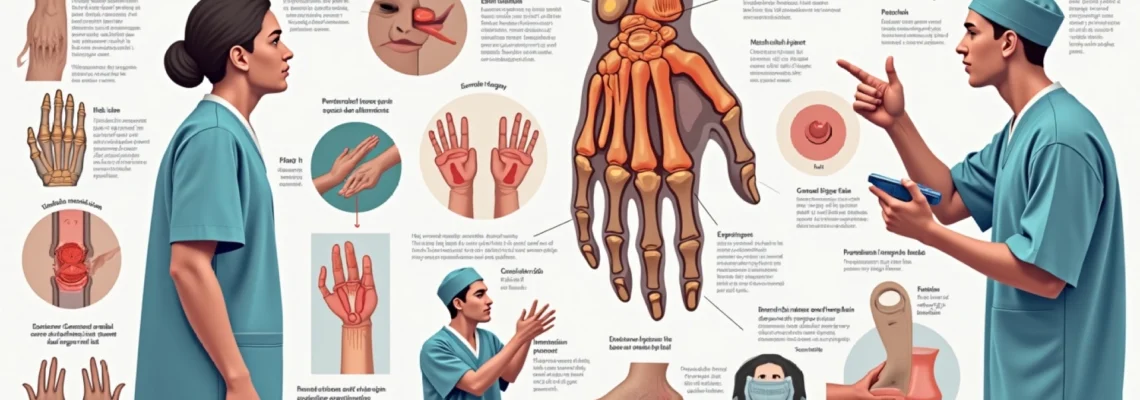
Ulnar shortening surgery represents one of the most challenging orthopaedic procedures when considering postoperative pain management and patient comfort. This surgical intervention, designed to address ulnar impaction syndrome and related wrist disorders, involves significant bone manipulation and soft tissue disruption that can result in considerable discomfort during recovery. Understanding the pain levels associated with this procedure is crucial for patients considering this treatment option, as well as healthcare providers managing postoperative care.
The complexity of ulnar shortening osteotomy stems from its invasive nature, requiring precise bone cuts, hardware installation, and extensive soft tissue manipulation around sensitive anatomical structures. Pain perception varies significantly among individuals , but clinical data consistently demonstrates that this procedure ranks among the more painful orthopaedic interventions. The multifaceted nature of pain following ulnar shortening surgery encompasses immediate postoperative discomfort, hardware-related irritation, and potential complications that can extend the pain experience well beyond typical recovery timelines.
Understanding ulnar shortening osteotomy: surgical procedure and pain mechanisms
Ulnar shortening osteotomy fundamentally involves removing a predetermined segment of the ulnar bone to reduce mechanical stress on the wrist joint. This procedure requires extensive surgical exposure, precise bone cutting techniques, and rigid internal fixation using plates and screws. The surgical trauma extends beyond bone manipulation to include significant soft tissue dissection, periosteal elevation, and potential nerve irritation throughout the operative field.
The pain mechanisms associated with this surgery are multifactorial, involving nociceptive pain from tissue damage, inflammatory responses at the surgical site, and potential neuropathic components from nerve manipulation. Understanding these pain pathways helps explain why patients experience varying degrees of discomfort and why traditional pain management approaches may not always provide adequate relief during the initial recovery phases.
Chevron osteotomy technique and tissue trauma assessment
The chevron osteotomy technique creates a V-shaped bone cut that requires extensive bone manipulation and hardware placement. This method generates significant periosteal stripping and bone marrow exposure, contributing to intense immediate postoperative pain. The tissue trauma associated with chevron cuts often results in prolonged inflammatory responses and delayed bone healing, which can extend the duration of significant pain beyond typical recovery expectations.
Oblique osteotomy method and nerve proximity considerations
Oblique osteotomy techniques position the bone cut closer to sensitive nerve structures, particularly the posterior interosseous nerve and superficial sensory branches. This proximity increases the risk of nerve irritation and subsequent neuropathic pain components. Patients undergoing oblique osteotomy frequently report shooting or burning sensations along the forearm, which can persist for months following surgery and contribute significantly to overall pain scores.
Wafer distal ulnar resection alternative and pain comparison
Wafer distal ulnar resection represents an alternative approach that removes bone from the ulnar head rather than the shaft. Comparative studies indicate that wafer procedures generally result in less immediate postoperative pain due to reduced hardware requirements and smaller surgical exposures. However, this technique may not provide equivalent long-term mechanical benefits, creating a challenging decision point between immediate comfort and long-term functional outcomes.
Dorsal radioulnar joint capsule disruption during surgery
Surgical access to the ulnar shaft often requires disruption of the dorsal radioulnar joint capsule, contributing to deep, aching pain that patients frequently describe as particularly troublesome. This capsular disruption can result in prolonged joint stiffness and pain with rotation movements. The capsular healing process typically requires 8-12 weeks, during which patients experience significant discomfort with forearm rotation and wrist positioning activities.
Postoperative pain intensity scale and clinical pain measurements
Clinical assessment of pain following ulnar shortening surgery relies on standardised measurement tools that capture both the intensity and quality of patient discomfort. These validated instruments provide crucial data for pain management protocols and help establish realistic expectations for patients considering this procedure. Research consistently demonstrates that ulnar shortening surgery produces some of the highest initial pain scores among upper extremity orthopaedic procedures.
Multiple studies report average pain scores exceeding 7 out of 10 during the first 48-72 hours postoperatively, with many patients experiencing peak pain levels of 9-10 during the immediate postoperative period. Pain intensity typically remains elevated for the first week , with gradual improvement occurring over 6-8 weeks as bone healing progresses and inflammatory responses subside.
Visual analogue scale (VAS) scores in first 72 hours
Visual Analogue Scale measurements consistently demonstrate severe pain levels during the initial recovery period following ulnar shortening osteotomy. Research data indicates average VAS scores of 8.2 ± 1.4 at 24 hours postoperatively, with minimal reduction to 7.8 ± 1.6 at 48 hours. These elevated scores reflect the significant tissue trauma and inflammatory response associated with the procedure.
Mcgill pain questionnaire results for ulnar shortening patients
The McGill Pain Questionnaire reveals that patients describe ulnar shortening surgery pain using terms such as “throbbing,” “aching,” “sharp,” and “burning.” The multidimensional nature of this pain experience indicates involvement of both nociceptive and neuropathic pain pathways. Affective pain descriptors suggest significant emotional impact, with many patients rating their pain as “exhausting” and “troublesome” during the acute recovery phase.
Numeric rating scale (NRS) pain documentation protocols
Numeric Rating Scale protocols for ulnar shortening patients typically involve hourly assessments during the first 24 hours, followed by regular monitoring throughout hospitalisation. Documentation reveals that pain levels rarely drop below 5/10 during the first week postoperatively, even with aggressive multimodal pain management approaches. These consistently elevated scores necessitate comprehensive pain management strategies and realistic patient counselling regarding expected discomfort levels.
Patient-reported outcome measures (PROMs) for wrist surgery
Patient-Reported Outcome Measures specifically designed for wrist surgery capture the functional impact of pain following ulnar shortening procedures. These instruments reveal that pain significantly impairs activities of daily living for 4-6 weeks postoperatively. The QuickDASH scores typically exceed 60 points during the first month, indicating severe functional limitations directly attributable to pain and discomfort.
Anatomical pain sources and nerve involvement during recovery
The anatomical complexity of the forearm and wrist region contributes significantly to the multifaceted pain experience following ulnar shortening surgery. Multiple tissue types undergo trauma during the procedure, each contributing distinct pain characteristics and recovery timelines. The surgical approach necessarily disrupts fascial planes, muscle attachments, and potentially sensitive nerve structures, creating a complex pain pattern that evolves throughout the healing process.
Bone pain represents the primary component during initial recovery, characterised by deep, aching discomfort that intensifies with movement or weight-bearing activities. The osteotomy site generates significant inflammatory responses that can persist for several months as bone healing progresses. Hardware-related pain emerges as a secondary concern , often manifesting as localised tenderness over plate and screw locations that may require eventual hardware removal in up to 45% of patients.
Nerve involvement varies depending on surgical technique and individual anatomical variations. The posterior interosseous nerve lies in close proximity to the ulnar shaft and can experience irritation or traction injury during bone manipulation. This nerve involvement may produce radiating pain patterns extending from the surgical site toward the wrist and hand. Additionally, superficial sensory nerve branches frequently sustain injury during surgical exposure, resulting in areas of numbness or hypersensitivity that can persist for months following surgery.
Soft tissue pain components include muscle spasm, fascial restriction, and joint stiffness that develop secondary to immobilisation and surgical trauma. The extensor muscle compartment often becomes particularly painful due to swelling and inflammation within the relatively confined fascial space.
The combination of bone, hardware, nerve, and soft tissue pain sources creates a complex clinical picture that requires multimodal management approaches for optimal patient comfort.
Pain management protocols and anaesthetic considerations
Effective pain management for ulnar shortening surgery requires comprehensive multimodal approaches that address the various pain mechanisms involved in this complex procedure. Regional anaesthesia techniques, including brachial plexus blocks and peripheral nerve blocks, provide excellent intraoperative anaesthesia and can significantly reduce immediate postoperative pain levels. These techniques offer the additional benefit of reducing opioid requirements and associated side effects during the critical initial recovery period.
Preemptive analgesia protocols incorporating anti-inflammatory medications, anticonvulsants for neuropathic pain components, and long-acting local anaesthetics can help establish better pain control foundations before surgical trauma occurs. Multimodal approaches consistently demonstrate superior outcomes compared to traditional opioid-based pain management strategies, particularly for procedures involving significant bone manipulation and hardware placement.
Postoperative pain management typically requires a combination of scheduled anti-inflammatory medications, acetaminophen, and carefully titrated opioid medications during the acute phase. The inflammatory component of pain responds well to regular NSAIDs when not contraindicated, while neuropathic pain elements may benefit from gabapentinoids or tricyclic antidepressants. Ice therapy, elevation, and early gentle range of motion exercises form important non-pharmacological components of comprehensive pain management protocols.
Patient-controlled analgesia systems can provide excellent pain control during hospitalisation, allowing patients to self-administer medications within prescribed safety parameters. However, the transition to oral medications often represents a challenging period where pain levels may temporarily increase.
Careful coordination between anaesthesia providers, surgeons, and nursing staff ensures seamless pain management transitions that minimise patient discomfort throughout the recovery process.
Recovery timeline and expected pain duration following ulnar shortening
The recovery timeline following ulnar shortening surgery follows predictable patterns, though individual variation exists based on factors including surgical technique, patient age, comorbidities, and compliance with rehabilitation protocols. Understanding these timelines helps establish realistic expectations and allows for appropriate pain management planning throughout the recovery process. Most patients experience their peak pain levels during the first 72 hours postoperatively, with gradual improvement occurring over subsequent weeks.
Week one typically involves severe pain requiring prescription pain medications and significant activity restrictions. Pain levels during this period often range from 6-9 out of 10, even with appropriate pain management protocols. Sleep disruption is common during this phase due to positional pain and difficulty finding comfortable sleeping positions. Daily activities remain severely limited, and patients require assistance with basic tasks involving the affected extremity.
Weeks two through six represent a transitional period where pain gradually decreases but remains significant enough to impact daily functioning. Many patients can transition from prescription opioids to over-the-counter pain relievers during this timeframe, though breakthrough pain episodes may still require stronger medications. Range of motion exercises begin during this period, often causing temporary increases in discomfort as healing tissues are mobilised. The bone healing process continues throughout this phase, contributing to ongoing deep, aching pain that gradually diminishes in intensity.
Months two through six mark the period where most patients achieve acceptable comfort levels for routine activities, though certain movements or activities may continue to provoke discomfort. Hardware-related pain may become more apparent during this phase as acute inflammatory responses subside. Approximately 25-45% of patients develop hardware irritation that requires eventual removal, typically occurring 6-12 months postoperatively once bone healing is complete. Weather changes, overuse activities, or prolonged positioning may trigger pain episodes throughout this extended recovery period.
Complication-related pain and Long-Term discomfort patterns
Complications following ulnar shortening surgery can significantly alter expected pain patterns and recovery timelines, creating additional challenges for both patients and healthcare providers. Non-union represents one of the most serious complications, occurring in approximately 8% of cases and resulting in persistent, often severe pain at the osteotomy site. This complication typically manifests as continued deep, aching pain that fails to improve beyond the initial weeks following surgery, often accompanied by increased pain with weight-bearing or rotational activities.
Hardware complications contribute substantially to long-term pain patterns, with studies indicating that up to 51% of patients experience some degree of hardware irritation. Plate prominence and screw irritation create localised areas of tenderness and discomfort that may worsen over time as overlying soft tissues become increasingly sensitive to the underlying metal structures. This hardware-related pain often develops insidiously, beginning as mild discomfort during certain activities and progressing to constant awareness or pain that interferes with daily functioning.
Chronic regional pain syndrome represents a devastating complication affecting approximately 6.7% of patients undergoing ulnar shortening surgery. This condition creates severe, disproportionate pain accompanied by autonomic dysfunction, skin changes, and functional impairment that extends far beyond the original surgical site. The pain associated with CRPS is often described as burning, crushing, or electric shock-like sensations that can spread throughout the entire extremity.
Early recognition and aggressive treatment of CRPS are essential for preventing permanent functional disability and chronic pain syndromes that can persist indefinitely.
Nerve injury complications, while less common, can create persistent neuropathic pain patterns that significantly impact quality of life. Posterior interosseous nerve irritation may result in deep, aching forearm pain accompanied by weakness in finger and thumb extension. Superficial sensory nerve injuries create areas of numbness, tingling, or hypersensitivity that can persist for months or years following surgery. These neuropathic pain components often respond poorly to traditional pain medications and may require specialised treatment approaches including nerve blocks, anticonvulsants, or topical agents for optimal management.