The peculiar sensation of fluttering in the ear can be one of the most disconcerting auditory experiences, often described as feeling like butterfly wings beating or helicopter blades whirring within the ear canal. This phenomenon affects millions of individuals worldwide, ranging from brief, intermittent episodes to persistent, life-altering conditions that significantly impact quality of life and hearing function. Understanding the complex mechanisms behind ear fluttering requires examining the intricate anatomy of the auditory system, where even minor disruptions can manifest as these distinctive vibratory sensations.
The causes of ear fluttering span a remarkably diverse spectrum of anatomical, neurological, vascular, and inflammatory conditions. From simple muscle spasms in the middle ear to complex arteriovenous malformations, each underlying cause presents unique challenges for both diagnosis and treatment. Modern medicine has revealed that what patients often dismiss as a minor annoyance can sometimes signal more serious underlying conditions requiring prompt medical attention. The challenge lies in distinguishing between benign, self-limiting episodes and those that warrant comprehensive investigation by healthcare professionals.
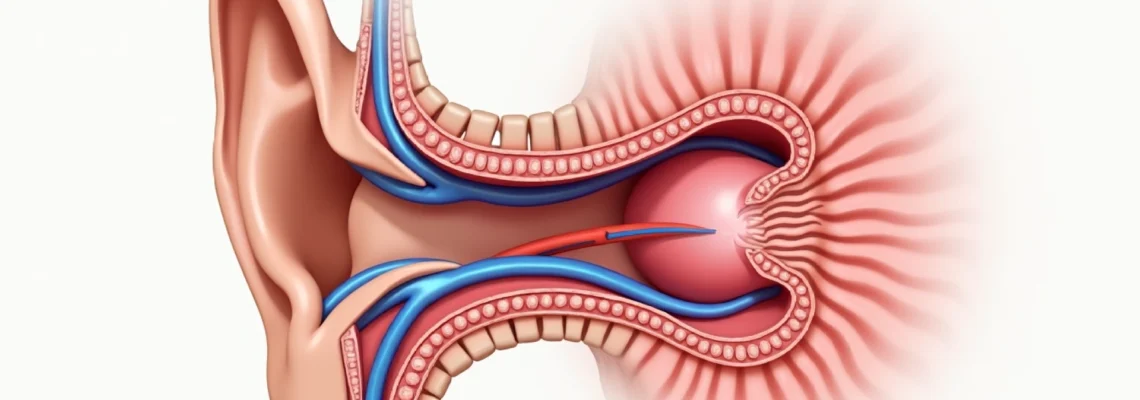
Anatomical origins of ear fluttering: tympanic membrane and middle ear dynamics
The middle ear represents a remarkable acoustic engineering marvel, where precise mechanical movements translate sound waves into neural signals. When examining ear fluttering from an anatomical perspective, the intricate interplay between the tympanic membrane, ossicular chain, and surrounding musculature becomes paramount. The middle ear cavity, roughly the size of a small marble, houses sophisticated mechanisms that can generate fluttering sensations when functioning abnormally.
Eustachian tube dysfunction and pressure equalisation mechanisms
Eustachian tube dysfunction stands as one of the most prevalent causes of ear fluttering, affecting approximately 4% of adults annually. This narrow passage, connecting the middle ear to the nasopharynx, serves as the primary mechanism for pressure equalisation across the tympanic membrane. When the Eustachian tube fails to open and close properly, pressure differentials create mechanical stress on the eardrum, resulting in characteristic fluttering sensations.
The pathophysiology involves impaired ventilation of the middle ear space, leading to negative pressure formation. This negative pressure can cause the tympanic membrane to retract inward, creating intermittent contact with middle ear structures. The resulting mechanical vibrations manifest as fluttering sounds that synchronise with breathing patterns, swallowing, or jaw movements. Inflammatory conditions, allergic rhinitis, and anatomical variations all contribute to Eustachian tube dysfunction.
Stapedius and tensor tympani muscle spasms
The stapedius and tensor tympani muscles, though microscopic in size, play crucial roles in protecting the inner ear from acoustic trauma. These muscles normally contract reflexively in response to loud sounds, but pathological spasms can occur spontaneously, creating rhythmic fluttering sensations. The stapedius muscle, measuring only 6.3mm in length, represents the smallest skeletal muscle in the human body yet can generate significant auditory disturbances when malfunctioning.
Middle ear myoclonus, characterised by involuntary contractions of these muscles, produces distinctive clicking or fluttering sounds that patients often describe as typewriter-like or resembling morse code . The condition can be idiopathic or secondary to neurological disorders, stress, caffeine consumption, or acoustic trauma. Electromyographic studies have documented muscle contraction frequencies ranging from 10-240 contractions per minute, correlating with the perceived fluttering intensity.
Ossicular chain displacement and conductive pathway disruption
The ossicular chain, comprising the malleus, incus, and stapes bones, forms the mechanical linkage between the tympanic membrane and inner ear. Displacement or fixation of these tiny bones can create abnormal vibratory patterns, manifesting as fluttering sensations. Otosclerosis, a condition affecting approximately 3% of the population, represents the most common cause of ossicular chain dysfunction in adults.
Traumatic disruption of the ossicular chain, whether from barotrauma, head injury, or surgical intervention, can result in intermittent mechanical instability. The displaced bones may intermittently contact surrounding structures, creating irregular vibratory patterns perceived as fluttering. Advanced imaging techniques, including high-resolution computed tomography, have revolutionised the diagnosis of ossicular chain pathology, enabling precise localisation of mechanical disruptions.
Tympanic membrane retraction and atelectasis
Tympanic membrane retraction occurs when chronic negative pressure in the middle ear causes the eardrum to collapse inward, potentially adhering to middle ear structures. This condition, known as atelectasis, can create intermittent fluttering as the membrane alternately adheres to and separates from underlying structures. The severity ranges from mild retraction pockets to complete adhesion to the promontory.
Chronic otitis media, particularly in childhood, predisposes individuals to tympanic membrane retraction in adulthood. The retracted membrane becomes hypermobile, responding to minor pressure changes with exaggerated movements that generate fluttering sensations. Treatment approaches vary from conservative management with nasal decongestants to surgical intervention including tympanoplasty or mastoidectomy.
Neurological conditions causing auditory flutter sensations
Neurological origins of ear fluttering encompass a complex array of conditions affecting cranial nerves, brain stem nuclei, and peripheral nerve pathways. The intricate neural control of auditory function means that disruptions at various levels of the nervous system can manifest as fluttering sensations, often accompanied by other neurological symptoms that provide diagnostic clues.
Myoclonus of the soft palate and palatial tremor
Palatial myoclonus represents a fascinating neurological condition where rhythmic contractions of the soft palate muscles create auditory disturbances, including ear fluttering. This condition affects the levator veli palatini and tensor veli palatini muscles, which have direct anatomical connections to the Eustachian tube mechanism. The myoclonic movements typically occur at frequencies of 1-3 Hz, creating characteristic clicking or fluttering sounds that patients can often hear themselves.
Essential palatial tremor, distinguished from symptomatic forms, often presents as an isolated finding without underlying brainstem pathology. Patients frequently report that the fluttering sensations intensify during periods of stress, fatigue, or emotional arousal. The condition can significantly impact sleep quality, as the rhythmic nature of the symptoms becomes more noticeable in quiet environments. Treatment options include anticonvulsants, muscle relaxants, and in severe cases, botulinum toxin injections.
Trigeminal neuralgia and cranial nerve V irritation
The trigeminal nerve’s extensive innervation of facial structures includes connections that can indirectly affect middle ear function. Trigeminal neuralgia, characterised by paroxysmal shooting pains, can sometimes present with atypical symptoms including ear fluttering. The nerve’s mandibular division provides motor innervation to the tensor tympani muscle, explaining the potential connection between trigeminal dysfunction and middle ear symptoms.
Atypical trigeminal neuralgia may manifest as burning, aching, or pressure sensations rather than the classic sharp, electric shock-like pains. These atypical presentations can include auditory symptoms such as fluttering, particularly when the auriculotemporal branch is involved. The temporal relationship between facial pain episodes and ear fluttering often provides crucial diagnostic information for healthcare providers.
Essential tremor affecting auricular muscles
Essential tremor, affecting approximately 1% of the population, can involve the small muscles surrounding the ear, creating fluttering sensations that patients often find difficult to describe. Unlike Parkinson’s disease tremor, essential tremor typically occurs during action or sustained postures, which may explain why some patients notice ear fluttering when lying down or during periods of concentration.
The auricular muscles, though vestigial in humans, retain innervation and can participate in generalised tremor disorders. Electrophysiological studies have documented tremor frequencies of 4-12 Hz in the auricular region, corresponding to the typical range of essential tremor. The fluttering sensations may be accompanied by visible tremor of the external ear, providing an important clinical sign for diagnosis.
Hemifacial spasm and facial nerve hyperexcitability
Hemifacial spasm, resulting from vascular compression of the facial nerve at the cerebellopontine angle, can create a cascade of symptoms including ear fluttering. The stapedius muscle, innervated by the facial nerve, becomes hyperexcitable, producing involuntary contractions that manifest as clicking or fluttering sounds. This condition affects approximately 8 per 100,000 individuals, with a female predominance.
The progression of hemifacial spasm typically begins around the eye and spreads to involve the entire ipsilateral face, including the stapedius muscle. Patients often report that the ear fluttering represents one of the most bothersome aspects of their condition, as it can occur independently of visible facial spasms. Microvascular decompression surgery has shown excellent results, with success rates exceeding 90% in appropriately selected cases.
Vascular causes: pulsatile tinnitus and arterial abnormalities
Vascular causes of ear fluttering represent a particularly important category, as they may indicate underlying cardiovascular conditions requiring urgent medical attention. The rich vascular supply to the temporal region and inner ear creates numerous opportunities for blood flow abnormalities to manifest as auditory symptoms. Understanding these vascular causes requires appreciating the complex relationship between systemic circulation and the delicate structures of the inner ear.
Carotid artery stenosis and turbulent blood flow
Carotid artery stenosis, affecting approximately 7% of individuals over 65 years, can create turbulent blood flow patterns that manifest as pulsatile ear fluttering. The carotid bifurcation’s proximity to the middle ear means that flow disturbances in this critical vessel can be transmitted to auditory structures. The fluttering typically synchronises with the cardiac cycle, creating a characteristic whooshing or fluttering sensation that intensifies during systole.
Atherosclerotic plaques in the carotid artery create flow acceleration and turbulence, generating acoustic energy that can be perceived as ear fluttering. The severity of stenosis correlates with the intensity of auditory symptoms, with critical stenosis (>70% diameter reduction) producing the most pronounced symptoms. Doppler ultrasound studies have documented the relationship between stenosis severity and audible bruits, providing objective correlation with patient symptoms.
Arteriovenous malformations in temporal region
Arteriovenous malformations (AVMs) in the temporal region represent rare but potentially serious causes of ear fluttering. These abnormal connections between arteries and veins create high-flow states that can be perceived as continuous or pulsatile auditory symptoms. Temporal region AVMs affect approximately 1 in 100,000 individuals, but their proximity to auditory structures makes them disproportionately likely to cause ear symptoms.
The characteristic feature of AVM-related ear fluttering is its continuous nature, often described as machinery-like or resembling rushing water . Unlike other vascular causes, AVM-related symptoms typically do not vary significantly with cardiac cycle or body position. Advanced imaging, including magnetic resonance angiography and digital subtraction angiography, has revolutionised the diagnosis and treatment planning for these complex vascular lesions.
Jugular bulb dehiscence and venous pulsations
Jugular bulb dehiscence occurs when the bony covering of the jugular bulb is absent or deficient, allowing venous pulsations to be transmitted directly to the middle ear. This anatomical variant affects approximately 6% of the population but only rarely causes symptoms. When symptomatic, patients experience pulsatile ear fluttering that intensifies with increased venous pressure, such as during Valsalva manoeuvres or coughing.
High-riding jugular bulb, another anatomical variant, can similarly cause venous pulsations to be perceived as ear fluttering. The symptoms typically worsen when lying down, as increased venous return enhances the pulsatile flow through the jugular system. High-resolution computed tomography has become the gold standard for diagnosing jugular bulb abnormalities, enabling precise anatomical assessment and surgical planning when intervention is required.
Hypertensive crisis and increased intracranial pressure
Severe hypertension and increased intracranial pressure can create vascular changes that manifest as ear fluttering. During hypertensive crises, systolic pressures exceeding 180 mmHg can cause arterial pulsations to become perceptible through bony conduction to the inner ear. The fluttering sensations typically accompany other symptoms of hypertensive crisis, including headache, visual disturbances, and altered mental status.
Increased intracranial pressure, whether from space-occupying lesions, hydrocephalus, or idiopathic causes, can similarly create vascular symptoms. The pressure elevation affects venous drainage patterns, potentially causing venous pulsations to become audible. Pseudotumor cerebri , particularly common in young, obese women, frequently presents with pulsatile auditory symptoms that patients describe as fluttering or whooshing sounds.
Inflammatory and infectious aetiologies of ear flutter
Inflammatory and infectious processes affecting the ear and surrounding structures represent common yet often underdiagnosed causes of ear fluttering. The middle ear’s susceptibility to inflammation stems from its communication with the upper respiratory tract through the Eustachian tube, creating pathways for infectious organisms and inflammatory mediators. Understanding these inflammatory causes requires recognising the complex interplay between local tissue responses and systemic inflammatory processes that can affect auditory function.
Acute otitis media, affecting over 80% of children by age three, can create temporary alterations in middle ear mechanics that manifest as fluttering sensations. The accumulation of inflammatory fluid behind the tympanic membrane alters its compliance and vibratory characteristics, creating abnormal acoustic transmission patterns. Even after successful antibiotic treatment, residual inflammation can persist for weeks, continuing to generate intermittent fluttering as tissue healing progresses.
Chronic otitis media with effusion presents a more insidious form of inflammatory ear pathology, where persistent middle ear fluid creates ongoing mechanical disturbances. The chronic nature of this condition means that fluttering sensations can persist for months or years, significantly impacting quality of life. The inflammatory process affects not only the middle ear space but also the Eustachian tube function, creating a cycle of poor ventilation and continued fluid accumulation.
Mastoiditis, though less common in the antibiotic era, remains a serious inflammatory condition that can cause ear fluttering through direct pressure effects on middle ear structures. The inflammatory process within the mastoid air cells can create pressure gradients that affect tympanic membrane movement, resulting in abnormal vibratory patterns. Modern imaging techniques have revealed that subclinical mastoiditis may be more common than previously recognised, potentially explaining some cases of unexplained ear fluttering.
External otitis, particularly the chronic forms, can create inflammatory changes that affect the ear canal’s acoustic properties. The swelling and debris accumulation alter sound transmission characteristics, potentially creating resonance effects that patients perceive as fluttering. Fungal otitis externa, increasingly common in humid climates, can produce particularly persistent symptoms due to the organism’s resistance to conventional treatments and tendency toward biofilm formation.
Mechanical obstructions and foreign body impaction
Mechanical obstructions within the ear canal or middle ear space represent readily treatable causes of ear fluttering that are frequently overlooked in clinical practice. The ear’s intricate acoustic design means that even small obstructions can create significant alterations in sound transmission and pressure dynamics. Understanding these mechanical causes requires appreciating how foreign materials interact with the ear’s natural cleaning mechanisms and acoustic properties.
Cerumen impaction affects approximately 10% of children and 5% of adults annually, making it one of the most common reversible causes of hearing impairment and ear symptoms. When cerumen accumulates against the tympanic membrane, it can create mechanical coupling that transmits external vibrations directly to the middle ear structures. The intermittent nature of cerumen-related fluttering often correlates with jaw movements, as mastication can alter the position of impacted wax relative to surrounding structures.
The composition and consistency of cerumen vary significantly among individuals, influenced by genetic factors, age, and environmental conditions. Wet cerumen
, commonly found in individuals of African and Native American descent, contains higher lipid concentrations that make it more prone to forming hard plugs. Dry cerumen, more prevalent in East Asian populations, tends to flake away naturally but can still accumulate in sufficient quantities to cause mechanical obstruction.
Foreign body impaction in the ear canal presents unique challenges, particularly in paediatric populations where curiosity often leads to insertion of small objects. Common foreign bodies include beads, insects, food particles, and cotton swab fragments. The mechanical irritation caused by these objects can create inflammatory responses that alter the ear canal’s acoustic properties, resulting in fluttering sensations that persist even after the foreign body is removed.
Insects trapped within the ear canal represent a particularly distressing form of mechanical obstruction, as their movement creates direct mechanical stimulation of sensitive ear canal tissues. The fluttering sensations caused by insect activity are often accompanied by intense discomfort and anxiety. Live insects can survive for extended periods within the ear canal, creating ongoing mechanical disturbance until professional removal is performed.
Otolith displacement, while primarily associated with vertigo, can occasionally manifest as fluttering sensations when calcium carbonate crystals become dislodged within the semicircular canals. These microscopic particles can create mechanical interference with normal fluid dynamics, resulting in abnormal sensory input that patients sometimes interpret as fluttering rather than the classic spinning sensation of vertigo.
Pharmacological triggers: ototoxic medications and drug-induced symptoms
Pharmaceutical agents represent an increasingly recognised cause of ear fluttering, with over 200 medications documented to possess ototoxic properties. The mechanism of drug-induced auditory symptoms varies considerably, ranging from direct cellular toxicity to alterations in neurotransmitter function. Understanding these pharmacological triggers becomes crucial as polypharmacy increases in aging populations, creating complex interactions that can manifest as auditory symptoms.
Aminoglycoside antibiotics, including gentamicin, tobramycin, and amikacin, are among the most well-documented ototoxic medications. These agents preferentially accumulate in the inner ear, where they interfere with mitochondrial protein synthesis in hair cells. The resulting cellular dysfunction can manifest as various auditory symptoms, including tinnitus and fluttering sensations. The risk of ototoxicity increases with cumulative dose, duration of treatment, and concurrent use of other ototoxic agents.
Loop diuretics, particularly furosemide and ethacrynic acid, can cause reversible ototoxicity through alterations in inner ear fluid composition. These medications affect the stria vascularis, disrupting the delicate ionic balance essential for normal auditory function. Patients receiving high-dose intravenous loop diuretics may experience acute onset of ear fluttering, typically resolving within hours to days of discontinuation.
Salicylates, including aspirin and methylsalicylate, produce dose-dependent ototoxicity that can manifest as ear fluttering at therapeutic doses exceeding 4-6 grams daily. The mechanism involves interference with prostaglandin metabolism within the cochlea, altering blood flow and cellular metabolism. Salicylate-induced auditory symptoms typically reverse within 72 hours of dose reduction or discontinuation, providing a useful diagnostic clue.
Chemotherapeutic agents, particularly platinum-based compounds like cisplatin and carboplatin, can cause progressive ototoxicity that may present initially as ear fluttering before progressing to more severe hearing loss. The cumulative nature of platinum ototoxicity means that symptoms may develop months after treatment completion, creating diagnostic challenges. Regular audiometric monitoring during and after chemotherapy has become standard practice to detect early signs of ototoxicity.
Antimalarial medications, including chloroquine and hydroxychloroquine, can cause ototoxicity through lysosomal accumulation and cellular dysfunction. The symptoms often develop insidiously over months to years of treatment, making the connection between medication and auditory symptoms less apparent. Patients with rheumatological conditions receiving long-term antimalarial therapy require periodic auditory assessment to detect early signs of ototoxicity.
Antiepileptic drugs, particularly phenytoin and carbamazepine, can occasionally cause ear fluttering through effects on neuronal excitability. These medications alter sodium and calcium channel function, potentially affecting the delicate neural control mechanisms of middle ear muscles. The temporal relationship between dose adjustments and symptom onset often provides important diagnostic information.
Benzodiazepines present a paradoxical relationship with ear fluttering, as they can both cause and treat the condition. While these medications can suppress muscle spasms that cause fluttering, they can also create withdrawal-related hyperexcitability that manifests as auditory symptoms. Patients experiencing benzodiazepine withdrawal may develop ear fluttering as part of a broader constellation of hyperexcitability symptoms.
Caffeine and other stimulants can trigger ear fluttering through effects on muscle excitability and anxiety levels. The relationship between caffeine consumption and ear symptoms often follows a dose-response pattern, with symptoms intensifying during periods of high intake and improving with reduction. Energy drinks containing multiple stimulants may produce particularly pronounced symptoms due to synergistic effects.
Topical medications applied to the ear canal, including certain antibiotics and antiseptics, can cause local irritation that manifests as fluttering sensations. Neomycin-containing ear drops are particularly problematic, as this antibiotic commonly causes contact dermatitis that can persist long after discontinuation. The inflammatory response alters ear canal mechanics, creating conditions conducive to abnormal acoustic transmission.
Recognising pharmacological triggers for ear fluttering requires careful medication history taking, including over-the-counter preparations, herbal supplements, and recreational substances. The temporal relationship between medication initiation, dose changes, and symptom onset provides crucial diagnostic information. Healthcare providers must maintain high suspicion for drug-induced causes, particularly in patients with multiple comorbidities requiring complex medication regimens.